Stomach Cells Rewired to Make Insulin: New Hope for Diabetes Treatment
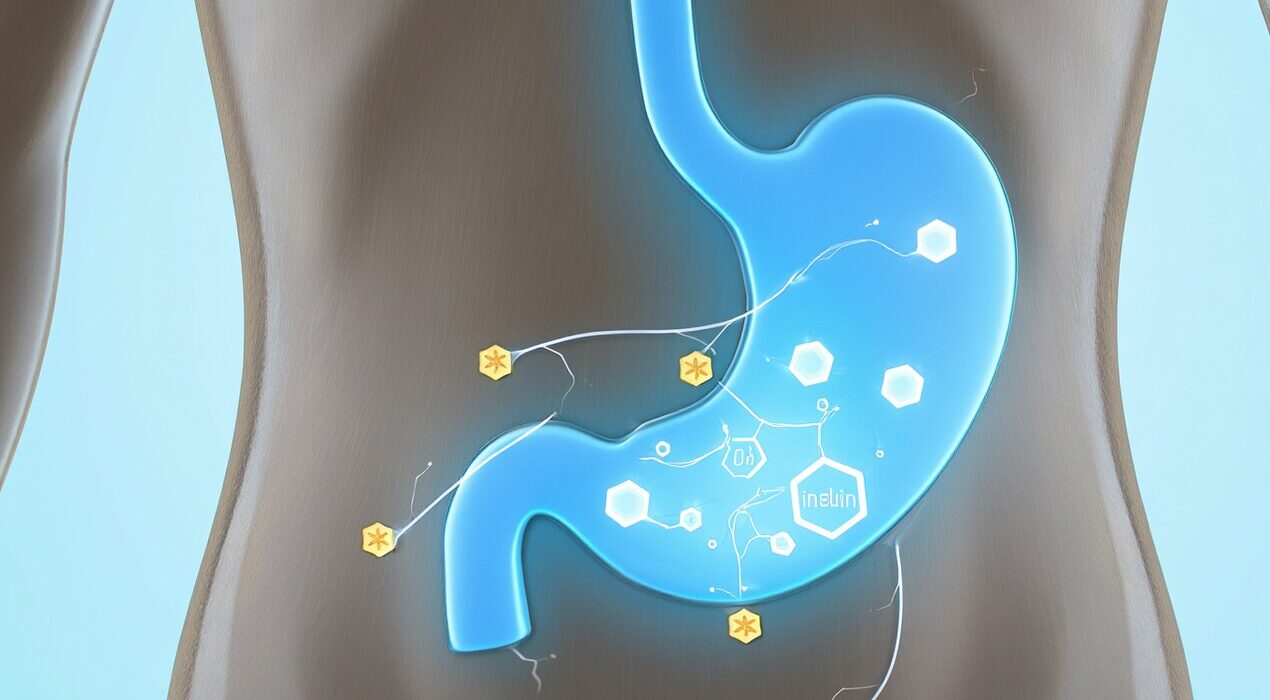
Scientists turned stomach cells into insulin-makers. In this new approach, human stomach cells were reprogrammed into cells similar to pancreatic beta cells. For example, in lab tests the modified cells produced insulin when glucose levels rose.
However, the work is still early. Researchers say this method must be tested further for safety and long-term effects. As a result, clinical use is still some years away.
How It Works & What It Means
The team used human stomach organoids,small tissue models of the stomach and applied a gene switch to convert them. These organoids then became insulin-secreting cells when transplanted in mice. When the switch flipped, they helped regulate blood sugar in diabetic mice.Therefore, this method could help people with diabetes one day. Instead of daily insulin injections, a person’s own stomach cells might make insulin internally.
In addition, the approach uses cells from the body already, which may reduce transplant rejection risks. But researchers emphasise more tests are needed before human trials.
Why This Matters
Diabetes, especially type 1, occurs when the body can’t make enough insulin because pancreatic beta cells fail. High blood sugar then damages organs like the eyes, kidneys and heart.By converting stomach cells into insulin-producers, we may repair or replace lost beta-cell function. This could shift treatment from simply managing blood sugar to actually restoring the body’s ability to respond to it.
Conclusion
In short, the key phrase “stomach cells insulin” sums up this study’s aim. While this development feels promising, the path ahead includes many steps. For now, it renews hope that future diabetes treatments could be more natural, integrated and less burdensome. Stay tuned for more progress.