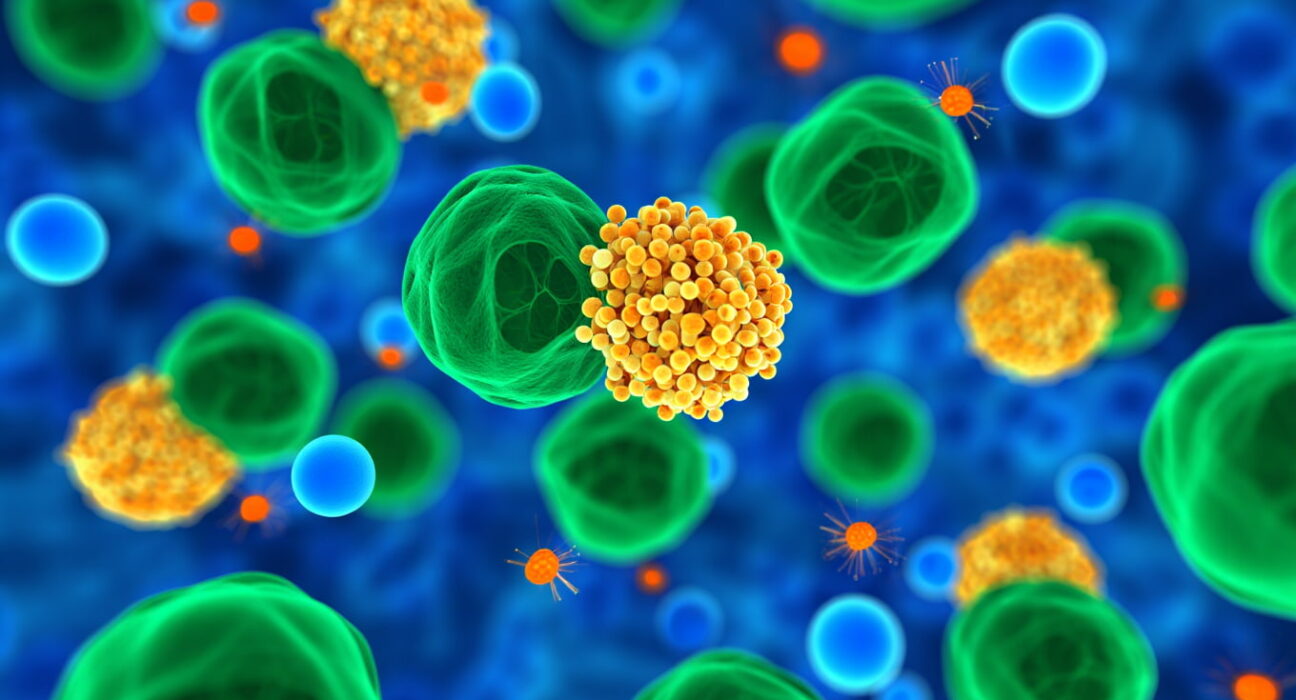
Metabolic-associated fatty liver disease (MASLD) affects nearly 30% of the global population and has long lacked targeted treatments. In a groundbreaking study, researchers have uncovered a genetic driver of the disease and identified vitamin B3 (niacin), an FDA-approved drug, as a promising therapeutic candidate.The discovery was led by Professor Jang Hyun Choi of UNIST, in collaboration with Professor Hwayoung Yun at Pusan National University and Professor Neung Hwa Park at Ulsan University Hospital. Their work highlights the role of microRNA-93 (miR-93), a small RNA molecule produced in liver cells, as a key regulator in MASLD development and progression.MiR-93 normally suppresses certain genes, but the team found it was abnormally elevated in both human patients with fatty liver and animal models. Elevated miR-93 blocked the activity of SIRT1, a gene crucial for controlling lipid metabolism. This suppression promoted fat accumulation in the liver, along with inflammation and fibrosis. In experiments, mice lacking miR-93 showed reduced liver fat, better insulin sensitivity, and improved liver health, while mice with high miR-93 levels experienced severe metabolic disruption.To explore therapeutic options, the team screened 150 existing FDA-approved drugs. Niacin (vitamin B3) emerged as the most effective at reducing miR-93 levels. In treated mice, niacin suppressed hepatic miR-93, restored SIRT1 activity, and normalized lipid metabolism, significantly improving liver function.The researchers emphasized that this study not only clarifies the molecular mechanisms underlying MASLD but also demonstrates the potential of repurposing an established vitamin compound for treatment. Since niacin is already widely used for managing hyperlipidemia and has a favorable safety profile, it could serve as a valuable therapy—possibly in combination with other drugs—targeting miRNA pathways in fatty liver disease.
Could a Simple Vitamin Reverse the World’s Most Common Liver Disease?